-
-
Featured Care Areas

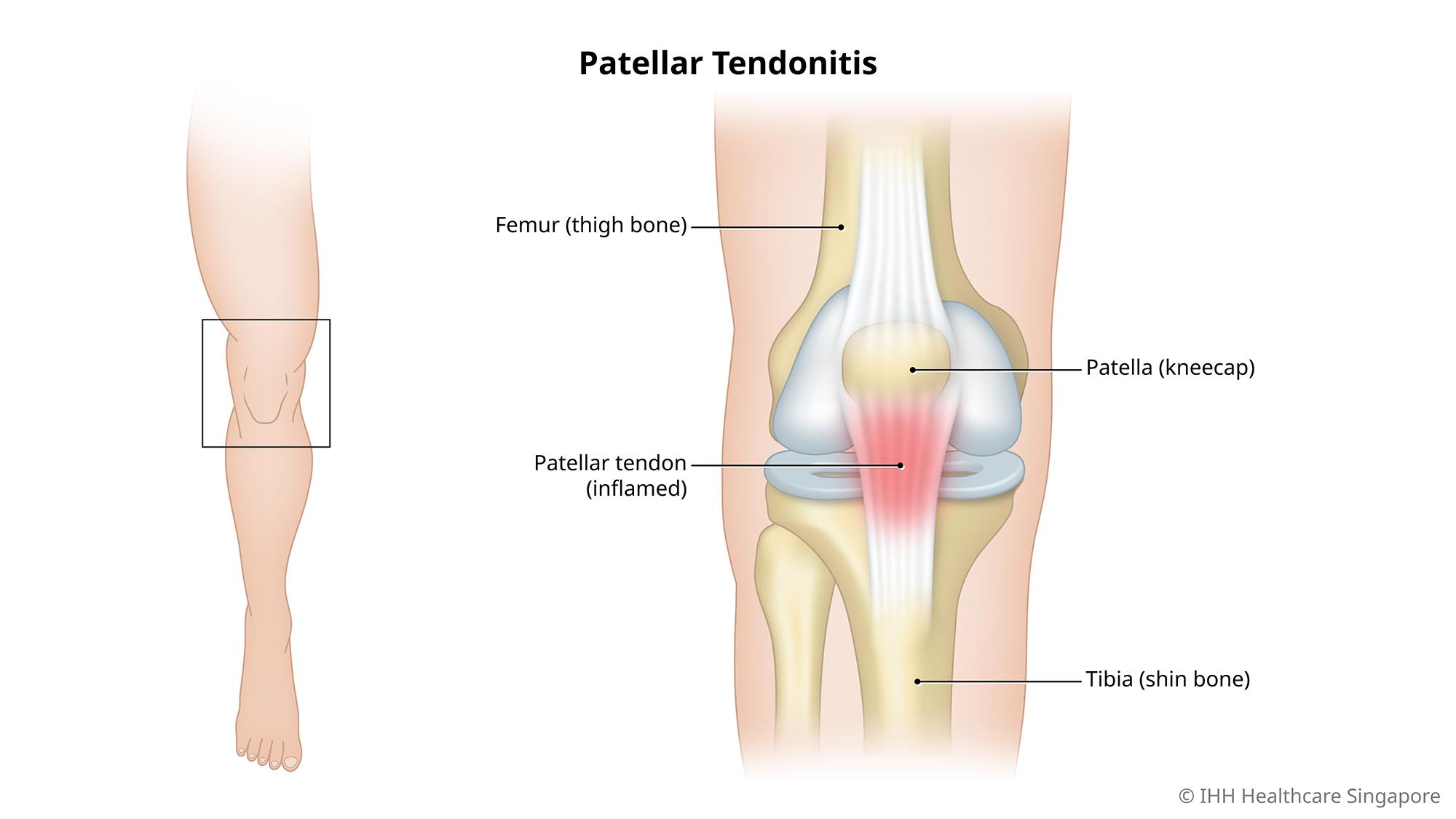
Patellar Tendonitis (Jumper's Knee)
What is patellar tendonitis (jumper's knee)?
Patellar tendonitis, also known as jumper’s knee, is an injury affecting the patellar tendon that connects the kneecap (patella) to the shin bone. The function of the patellar tendon is to assist the muscles during movement of the lower leg, in actions such as jumping, kicking and pedalling.
Patellar tendonitis is characterised by pain and inflammation which weakens the tendon, creating small tears. The resulting pain can interfere with daily activities, such as climbing stairs or sitting in a car, as well as sports activities.
What are the symptoms of patellar tendonitis?
Patellar tendonitis symptoms include:
- Pain and tenderness at the base of the kneecap, especially while kneeling or getting up from a squatting position
- Sporadic pain that worsens as the damage to the tendon gets worse
- Swelling or burning sensation in the kneecap
- Bruising or redness, especially if there has been an injury
- Discomfort from daily activities that require bending and straightening of the knee
What causes patellar tendonitis?
Patellar tendonitis (jumper's knee) is usually caused by overuse of the knee joint and repeated stress on the patellar tendon. It is more common among people who play sports that involve squatting and jumping movements such as basketball and volleyball.
What are the risk factors for patellar tendonitis?
Patellar tendonitis risk factors include:
- Tight thigh and hamstring muscles, which can increase the strain on the patellar tendon.
- Uneven leg muscle strength or muscular imbalance, with stronger muscles pulling harder on the patellar tendon.
- Abnormal alignment of the legs, ankles and feet, including conditions such as bow legs, knock knees and flat feet.
- Increased tension in the patellar tendon, which can occur when tendon growth cannot keep up with the growth of the lower leg. This is known as Sinding-Larsen-Johansson disorder, where the tendon pulls on the bottom tip of the kneecap.
- Obesity, which places increased pressure on the knee joint.
- Chronic illness such as kidney failure, rheumatoid arthritis or diabetes which can affect blood flow to the knee and weaken the tendon.
- Poor jumping and landing technique, due to the way the quadricep muscles contract.
How do you prevent patellar tendonitis?
You can reduce your risk of jumper's knee by:
- Stretching and warming up thoroughly before exercise
- Cooling down and stretching after exercise
- Wearing knee support devices while playing sports
- Strengthening the leg muscles that support the knees
- Practicing good technique while jumping and especially while landing
- Avoiding jumping or landing on hard surfaces such as concrete
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6250 0000 (Orchard) or +65 6898 6898 (Novena)
For appointment bookings, please WhatsApp
+65 8111 7777 (Orchard) or +65 8111 5777 (Novena)