-
-
Featured Care Areas

Slipped (Herniated) Disc
What is a slipped disc?
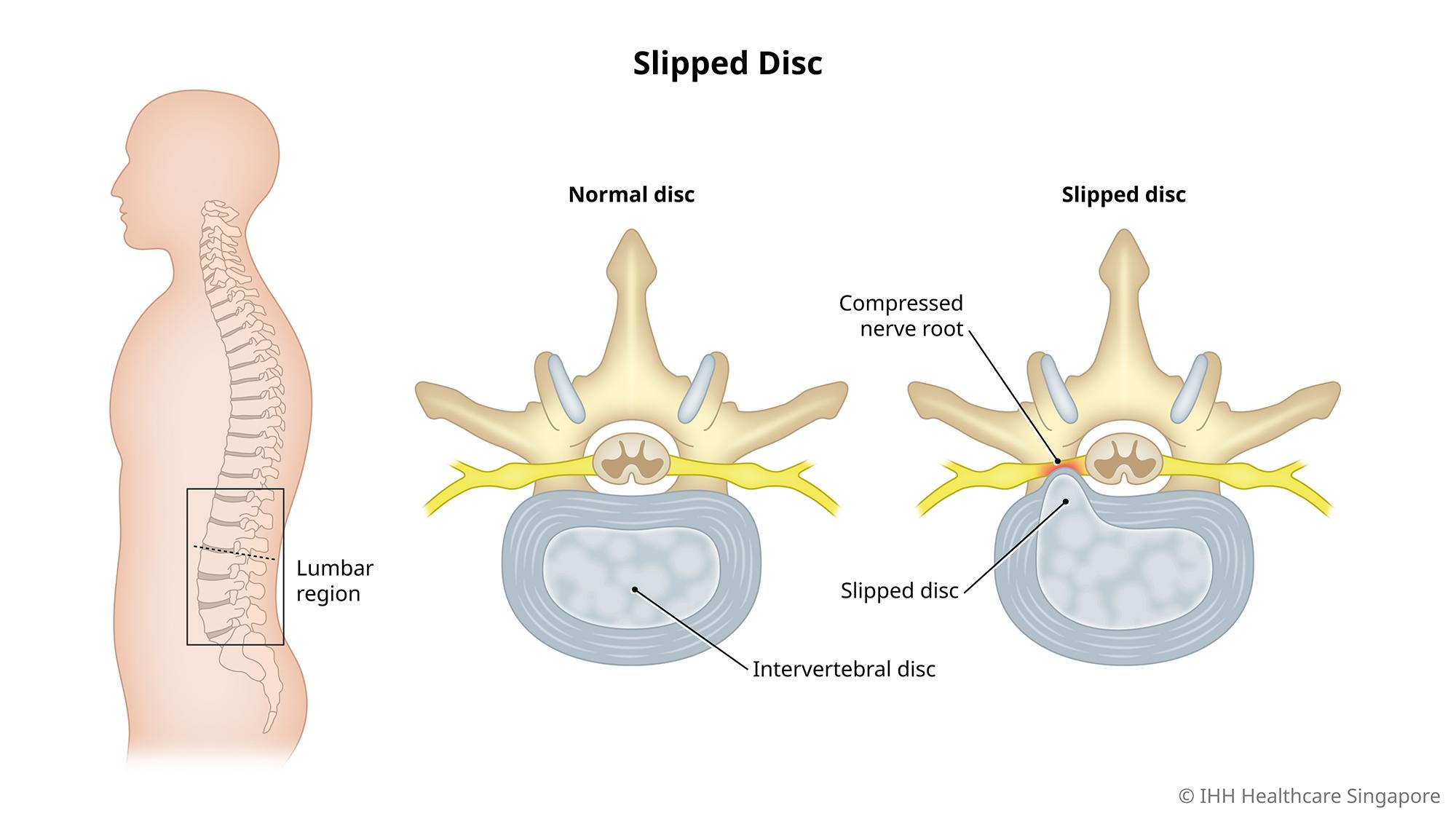
Discs are located between each vertebra of the spine to keep the spine supple and absorb the shock or impact of daily activities.
A slipped disc occurs when the outer covering of the disc (annulus) tears and the internal gel filling (nucleus pulposus) gets pushed out of the covering (herniates), causing the gel to press on the nerve root.
This condition is also known as a ‘herniated’, ‘ruptured’ or ‘prolapsed’ disc.
What are the symptoms of a slipped disc?
Symptoms of a slipped disc vary depending on where the affected disc is and whether the disc is pressing on a nerve. These include:
- Numbness or pain that starts from the lower back and shoots down the buttock or legs (sciatica)
- Numbness or tingling that radiates from the body part served by the affected nerves
- Pain in buttocks, thigh, calf, and part of the foot
- Sharp or burning pain in the shoulder and arm that may shoot to the arm or leg when coughing, sneezing or moving into certain positions
- Weakness in muscles that cause stumbling, or affects the ability to lift or hold items
- Difficulty controlling bowel movements and urination
- Numbness in the genitals and anus
A herniated disc usually causes more pain compared to a bulging disc.
It is not always easy to differentiate between discomfort caused by a muscle strain and pain caused by a slipped disc. Discomfort from a backache or muscle strain usually goes away within 6 weeks, while pain caused by a slipped disc may progressively worsen.
What causes a slipped disc?
The main cause of a slipped disc is gradual wear and tear. As you age, your discs lose their elasticity and become more prone to damage or rupture with even a minor strain or twist.
Any activity that puts pressure on the spine may lead to a slipped disc. This can happen in the event of:
- Injury from lifting heavy objects incorrectly (e.g. using the back muscles instead of the leg and thigh muscles to lift heavy objects)
- Traumatic events. In rare occasions, a fall or blow to the back can result in a slipped disc.
What are the risk factors for a slipped disc?
The following factors can increase the risk of a slipped disc:
- Ageing. Slipped discs are most common in people aged 30 – 50 years, with men being twice as likely to experience a slipped disc.
- Genetics. People with a family history of slipped discs are likely to have a genetic predisposition for the condition.
- Occupation. Jobs which are strenuous and physically demanding increase the risk of a slipped disc.
- Poor posture. Poor posture while exercising or sitting for long periods can contribute to a slipped disc.
- Smoking. Nicotine and other toxins from cigarettes and tobacco products prevent absorption of nutrients by the discs, which in turn accelerates disc degeneration and contributes to further disc damage.
- Weight. Increased body weight causes extra stress on the discs in your lower back.
What are the complications and related diseases of a slipped disc?
As pain from a slipped disc worsens over time, many people tend to seek medical advice only when:
- The pain becomes intolerable
- Other symptoms such as incontinence or partial paralysis appear.
Left untreated, a slipped disc may lead to complications such as:
- Worsening symptoms, such as increased pain, numbness or weakness that can affect your daily routine.
- Loss of bladder control or bowel control, which may lead to incontinence or difficulty urinating even with a full bladder.
- Saddle anaesthesia, where the slipped disc compresses the nerves and leads to loss of sensation in the inner thighs, back of the legs and around the rectum.
- Permanent nerve damage, which may lead to permanent weakness or paralysis. Delays in diagnosis and treatment can permanently damage the nerves affecting the bladder, bowel and legs.
How do you prevent a slipped disc?
There are several steps you can take to prevent a slipped disc:
- Exercise. Exercises that strengthen the trunk muscles are helpful to stabilise and support the spine.
- Good posture. Practise good posture to reduce pressure on the spine and discs. When sitting, keep your back straight and aligned. Lift heavy objects by bending your hips and knees and not by bending forward.
- Healthy weight. A healthy weight reduces pressure on your spine and discs.
- Quit smoking. Discs stay hydrated and pliable longer without the toxins from cigarettes depriving them of vital nutrients.
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6250 0000 (Orchard) or +65 6898 6898 (Novena)
For appointment bookings, please WhatsApp
+65 8111 7777 (Orchard) or +65 8111 5777 (Novena)