Dr Ngaserin Sabrina Ng Hui Na
General Surgeon


Source: Shutterstock
General Surgeon
Breast cancer is the most common cancer among women in Singapore.
According to the Singapore Cancer Registry Annual Report 2023, breast cancer is the most common cancer among women, accounting for 29.9% of cases), presenting a lifetime risk of 8.6% (1 in 12). It is also a leading cause of cancer deaths in women (17.9% of cancer deaths among females).
Breast cancer occurs most commonly in women between the ages of 40 to 69 years, however 1 in 6 cases are diagnosed in younger women aged 45 years and below. Breast cancer can affect anyone, even younger women with no obvious risk factors. This is why all women above the age of 20 are encouraged to do monthly breast self-examinations to pick up any signs of abnormal changes in their breasts.
If you do find a breast lump during your breast self-examination, there is no need to panic. Many breast lumps often turn out to be benign (non-cancerous). But to be on the safe side, you should consult a breast care specialist who may suggest diagnostic breast imaging, such as mammography, ultrasonography, or sometimes breast MRI, for further evaluation.
For women without symptoms (asymptomatic), annual screenings mammograms are highly encouraged starting from the age of 40. Studies show that mammograms can help in the early detection of breast cancer, even before any breast lumps can be felt, and timely treatment may reduce the extent of therapy required and improve overall survival.
Just like how everyone's personality is unique, your breasts, too, are the same. Some women have naturally lumpy breasts. Hormonal changes, breastfeeding, and the natural process of ageing can also cause changes in the way your breasts look and feel.
What's important is to regularly self-examine your breasts every month, ideally within 7 – 10 days after your menstrual period starts when the breasts are least tender and swollen, so you can look out for any unusual changes in your breasts. For menopausal women, select an easy day to remember, such as the first day of each month.
Some warning signs that might indicate breast cancer include:
All unusual findings should be evaluated by an experienced healthcare professional.
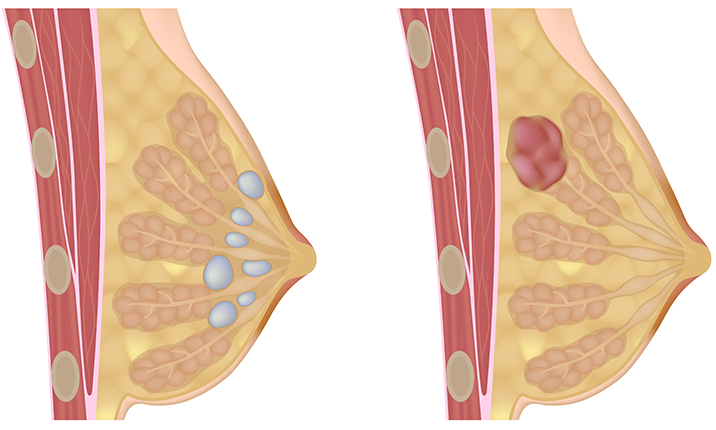
There are many different causes of breast lumps. Most of them are benign and can be caused by tissue growth (like fibroadenomata and fibrocystic change) or a build-up of fluid (like a cyst). A cancerous lump, however, most commonly presents as a painless lump, and can start small before it enlarges with time.
Hence if you find any lumps in your breast, the best thing to do is schedule a visit to a breast specialist to seek reassurance or establish an early diagnosis.
It’s important to emphasise: you cannot reliably tell whether a lump is cancerous just by feel alone.
However, there are certain features that tend to raise suspicion. Below is a comparison of typical benign vs suspicious (cancerous) characteristics. These are guidelines, not guarantees.
| Feature | Benign (more likely) | Suspicious / Cancerous (more concerning) |
|---|---|---|
| Texture / Firmness | Soft, rubbery, or somewhat compressible | Hard, firm, dense, may feel “rock-like” |
| Edges / Shape | Smooth, well-defined, regular margin | Irregular, spiculated, ill-defined margins |
| Mobility (movable vs fixed) | Moves slightly under the skin (mobile) | May be fixed, immobile, tethered to skin or deeper tissues |
| Pain / Tenderness | Sometimes tender (especially related to hormone cycles or cysts) | Often painless (though not always) |
| Growth Over Time | Slow, stable, may fluctuate with menstrual cycle | May grow over time, become larger or firmer |
| Associated Features | No skin changes, no nipple changes | Skin changes (dimpling, puckering, redness, “orange peel” texture), nipple retraction, abnormal nipple discharge |
In summary, a hard, firm, irregular, and non-movable lump (especially one that does not change or goes away) is more suspicious.
The earliest signs of breast cancer are often subtle, such as textural changes in the breast, before a lump becomes noticeable. As the disease progresses, patients may develop dimpling, pitting, redness, ulceration of the skin or nipple area, or nipple discharge - particularly concerning if it is bloody, spontaneous and persistent.
Any new or changing lump or symptoms in the breast and nipple-areolar region should prompt evaluation.
Any new breast lump should be checked by an experienced healthcare professional.
If you have a personal or family history of breast cancer or identified genetic risk (e.g. BRCA mutations), be more vigilant.
About 10% of all breast cancer cases in Singapore are still being consistently diagnosed at Stage 4 disease - a proportion noticeably higher than in other developed countries.
Don’t delay evaluation out of fear; early diagnosis offers the best chance for effective treatment.
For benign lumps such as cysts / fibrocystic changes:
Specialist review is advised to ascertain if lesions and findings can be conclusively diagnosed as benign. Doctors will correlate clinical findings with breast imaging and sometimes tissue biopsy is utilised to confirm the diagnosis when in doubt.
There is no strong evidence that any herbal remedy, supplement, or home remedy can reliably “cure” or eliminate either benign or suspicious or cancerous lumps. Non-conventional or home remedies are anecdotal and unproven.
Danger of “natural cure” claims
All breast lumps should be evaluated by an experienced professional. Your doctor will correlate the clinical findings with imaging tests, such as mammogram or breast ultrasound. If the abnormality is indeterminate or suspicious, your doctor will decide if there's a need for further investigations such as tissue sampling (needle biopsy).
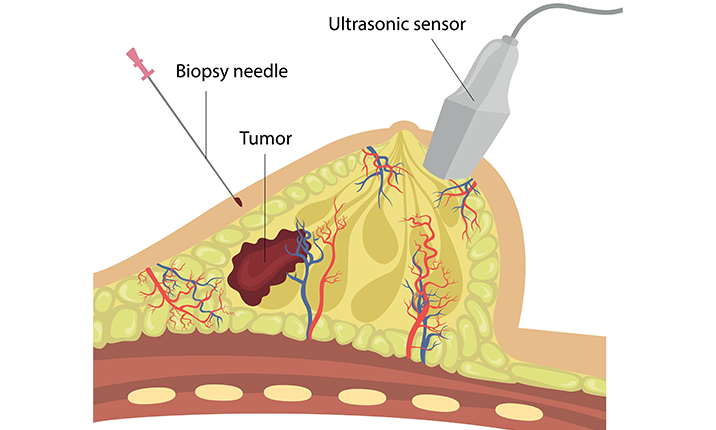
Biopsy techniques that are commonly used include: Image-guided core biopsy, image-guided vacuum assisted biopsy, and image-guided vacuum assisted excision. Vacuum assisted techniques are often diagnostic and therapeutic, as they typically aim for complete lesion removal.
In general, women are advised to start monthly breast self-examinations from the age of 20, paying attention to any changes in size, shape or appearance of the breast, the overlying skin, nipple and areolar, or axillary region (armpit).
That said, the superior strategy is not to wait for symptoms to arise, but to detect, diagnose and treat breast cancers at early or even pre-invasive stages, even before any masses develop, even before there are symptoms or signs, when the disease cannot be seen or felt.
The Singapore Cancer Society recommends regular screening mammograms.
With this strategy, breast specialists are often able to detect precursor or premalignant diseases and conditions at this stage can be better addressed with minimally invasive strategies that minimise disruption to life.
2D mammography is the most discussed screening modality because it is the recognised gold standard tool for breast cancer screening. Digital 2D mammograms capture 2-dimensional images of each breast.
Doctors also rely on other screening tests for detecting breast cancer, such as:
Breast cancer screening recommendations should be personalised based on individual risk. Breast cancer risk assessment tools use statistical models to estimate a woman’s risk of developing breast cancer over the next 5 years as well as over her lifetime.
A person is said to be of ‘average risk’ of developing breast cancer if this risk is 15% or under. By definition, high risk’ means greater than or equal to 20% lifetime risk, or in other words, a 1 in 5 chance of developing breast cancer over a lifetime.
About half of women of screening age have dense breast tissue, and specialists would strongly encourage women to recognise their own breast density when considering their imaging options. This helps ensure the most accurate detection and the best possible approach to early diagnosis.
For women at average risk, regular screening mammography is recommended starting at age 40. Those with a family history of breast cancer should begin screening 10 years earlier than the age at which their youngest affected relative was diagnosed.
A screening mammogram involves X-ray images of the breasts. It is not an invasive study and does not pose direct harm to one’s health. The radiation dose is extremely low, similar to natural background exposure over about 7 weeks, or a few transatlantic airplane flights, and has never been shown to cause harm.
In preparation for a screening mammogram, you will be asked some basic questions about your health before proceeding to the imaging area for your mammogram examination.
During the examination, you will be asked to undress to the waist before stepping up to the mammogram machine. The machine will gently compress each of your breasts between two plastic plates for a few seconds. Brief compression during a mammogram is necessary to evenly spread the breast tissue apart and obtain the clearest possible image. Two X-rays will be taken for each breast – one from top to bottom and one in an oblique angle.
If any abnormalities are detected, you may schedule an appointment with our doctors for further evaluation.
If an abnormality is detected during your screening mammogram, your doctor may suggest further imaging investigations to better visualise the lesions. For indeterminate or suspicious findings, a biopsy may be required to confirm if the tissue in your breast is high risk or cancerous. A biopsy is a simple medical procedure that involves extracting a tissue sample from your breast so that it can be assessed under a microscope in the laboratory for cancer. It will take several days to a week for the laboratory results to be confirmed.
If the results are negative for malignancy, that means good news - no sign of breast cancer. Your doctor will advise if you need any additional follow-up and when you should have your next screening or surveillance.
If the biopsy results are positive for cancerous cells, your breast specialist will be in the best position to immediately advise you on the recommended treatment plan.
Safeguard your health by going for regular mammogram screenings. While breast lumps are a hallmark symptom of breast cancer, they start small and may not be noticeable or detectable by touch, especially if they are pre-cancerous or when they are in the early stages of cancer. An increasing proportion of women diagnosed with breast cancer these days have no symptoms at all. Discovering breast cancer when abnormalities were picked up during their mammogram test means early detection and a greater chance of cure.
Most breast cancer patients in Singapore are diagnosed at early stage (stage 1 and 2) and have very good prognosis. The good news is that with early diagnosis and appropriate treatment, most breast cancer patients can achieve good long-term survival.
Treatment of breast cancer is a multidisciplinary and multimodality effort, and evolving evidence continues to refine modern breast cancer strategies.
Specialists involved in breast care include, but are not limited to breast surgeons, radiologists, pathologists, medical oncologists, radiation oncologists, plastic and reconstructive microsurgeons, breast nurses, physio and occupational therapists, are more. More women are benefiting from breast-conserving strategies, oncoplastic surgery, and minimally invasive surgical options, which aim to eradicate disease while optimising cosmetic outcomes.
When cancer is detected early and is proportionately small compared to the volume of the entire breast, breast-conserving surgery (BCS) is often the preferred approach for eligible patients. BCS removes cancer while preserving as much of the healthy breast tissue as possible.
In contrast, a mastectomy, or whole breast removal, may be necessary for more extensive disease, extremely high lifetime risk, or patient preference. For patients undergoing mastectomy, preservation of skin and the nipple-areolar complex, along with consideration of breast reconstruction, are essential components of care.
Oncoplastic breast surgery incorporates plastic surgery principles to perform breast volume displacement, replacement, reduction, or partial reconstruction, optimising cosmetic outcomes.
Minimally invasive breast surgery (MIBS), also known as keyhole surgery, is a relatively newer technical approach. Conventional breast surgery often leaves scars on the breast, nipple, areola, or lengthy scars along the bra line or lateral breast. In MIBS, surgeons use a digital endoscope with a fibre optic cable, video camera, and light or robotic surgery platforms within an air-insufflated surgical space to visualise the operative field with high precision. MIBS allows the removal of breast and cancerous tissue and perform reconstructions with small discrete scars, fine instruments, offering aesthetic benefits through concealed incisions, less pain, minimal scarring, and reduced risk of nipple, skin, and wound complications.
Seeking medical attention early can make a big difference in the treatment and recovery from breast cancer. Be vigilant, screen regularly, take subtle changes seriously, and consult the appropriate healthcare professional promptly when concerns arise. Don't hesitate to speak to a doctor should any changes in your breasts be noticed, or if you have questions about your breast health.
At Mount Elizabeth, we provide comprehensive cancer care delivered by a compassionate and experienced team of general surgeons, medical oncologists, and radiation oncologists. If you're experiencing breast cancer symptoms or have any health concerns, we’re here to help.
Find a specialist