Nutrition & Dietetics
Our Services
Dietetics and nutrition services
Our dedicated team of dietitians works closely with a multidisciplinary network of doctors and healthcare professionals to deliver integrated, personalised nutrition care. We support patients across a wide range of conditions, offering guidance and interventions that aid treatment, recovery, and long-term health.
Diet and nutrition programmes
We offer structured programmes built on evidence-based nutrition principles, tailored to individual dietary needs and health objectives. These programmes help patients develop sustainable eating habits, tackle specific nutritional challenges, and manage medical conditions effectively. Key focus areas include:
Chronic disease management
Good nutrition is essential for living well with long-term conditions. This programme provides personalised meal plans, practical advice, and ongoing guidance to help manage symptoms, support health, and reduce the risk of complications. We provide nutritional guidance for conditions such as:
Diabetes
- Balance carbohydrates, protein, and fat through personalised meal planning
- Portion control, carbohydrate counting, and following a low glycemic index (GI) diet for diabetics
- Healthy snacking and eating-out strategies
- Aligning meals with medication to support stable blood glucose
Hypertension and heart disease
- Reduce sodium through label reading and ingredient swaps
- Limit saturated and trans fats; increase heart-healthy fats and fibre
- Weight management support
- Integrated meal planning for multiple risk factors
Gastrointestinal disorders
- Identify and manage trigger foods that commonly affect people with irritable bowel syndrome and gastroesophageal reflux disease
- Provide guidance on low FODMAP and elimination diets to help reduce symptoms of irritable bowel syndrome
- Provide gluten-free diet guidance for managing coeliac disease
- Address nutritional deficiencies and support gut health for those with inflammatory bowel disease
Renal (kidney) conditions
- Manage chronic kidney disease (CKD) with diet guidance based on your glomerular filtration rate (GFR), dialysis nutrition, or kidney stone prevention
- Low-protein diet planning and electrolyte balance, such as potassium and sodium
- Helps keep your muscle and strength up during dialysis treatment
- Caregiver education for kidney-friendly meal preparation
Chronic liver conditions
- Provide nutritional guidance for fatty liver, liver detox, and other chronic liver conditions
- Tailor meal plans to manage liver function and support overall health
- Offer practical strategies to meet protein, vitamin, and mineral needs safely
Weight and obesity management
Maintaining a healthy weight can improve energy levels, lower the risk of chronic diseases, and enhance overall wellbeing. This programme offers personalised nutrition plans tailored to your lifestyle and health needs, with a focus on realistic and sustainable weight goals. Whether your aim is weight loss or preventing weight regain, we prioritise building lasting, healthy habits through:
- Balanced eating plans tailored to your lifestyle, preferences, and medical conditions
- Practical guidance on portion control and mindful eating
- Meal planning and grocery shopping tips
- Strategies to manage emotional eating and support behaviour change
- Ongoing support for long-term weight maintenance
Nutrition for cardiac rehabilitation
Nutrition plays an important role in recovery after a heart condition or cardiac procedure. This programme aims to improve cardiovascular health, aid recovery, and help prevent future complications as part of a comprehensive rehabilitation plan. We provide:
- Heart-healthy meal plans focused on reducing sodium, cholesterol, and unhealthy fats
- Strategies for increasing fibre and antioxidant intake
- Individualised nutrition guidance to support recovery alongside with exercise and medication
Feeding workshops and clinics for children
Introducing solids safely and confidently lays the foundation for balanced growth and development while reducing the risk of feeding difficulties and picky eating. Our feeding workshops and clinics support parents and caregivers of babies aged six months and above by providing clear guidance, practical strategies, and personalised advice to make this transition smooth and positive. The programme covers:
- Step-by-step guidance on when and how to start solids
- Identifying age-appropriate textures and food progression
- Strategies to encourage self-feeding and prevent picky eating
- Nutritional advice to ensure balanced meals for infants
- Support for feeding difficulties and growth concerns
- Tips for establishing positive, stress-free mealtimes and nurturing healthy eating habits from the start
Nutritional support for patients with cancer
Cancer and its treatments often present significant challenges to nutrition, appetite, and energy levels. To support you through these, our programme offers comprehensive care at every stage of the cancer journey, from diagnosis and active treatment to recovery and beyond. This programme supports patients who:
- Have been recently diagnosed with cancer
- Are experiencing unintentional weight loss (≥5% over 1 to 3 months)
- Are undergoing chemotherapy, radiotherapy, or immunotherapy
- Are preparing for surgery or recovering post-operation
- Are struggling with nutrition-related side effects of treatment
- Are concerned about nutrition myths or misinformation
- Are planning for long-term cancer survivorship
- Are unsure about what supplements to take or avoid
Severe weight loss and malnutrition can impact the function of vital organs, making it especially important to maintain good nutrition - particularly during surgery recovery or cancer treatment. Our dietitians provide tailored meal plans, including low residue diets for patients with digestive sensitivities, to help sustain energy, maintain a healthy weight, manage side effects, and support overall recovery.
Our programme helps with:
- Managing symptoms that affect food intake, including nausea, dry mouth, sore throat, fatigue, diarrhoea, constipation, and changes in taste or smell
- Maintaining adequate energy, protein, and fluid intake to prevent malnutrition and muscle loss
- Offering guidance on food safety, hydration, and nutrition to support the immune system
- Tailoring meal plan to address unintentional weight loss or gain and meet your nutrition goals
- Providing post-treatment nutrition strategies to support tissue repair, strength, and long-term wellbeing
- Advising on supplements and managing nutrition alongside chronic medical conditions
- Supporting caregivers with meal preparation advice, feeding advice, and encouragements.
If you’re unsure about your current nutritional status, take a moment to assess your well-being with this Malnutrition Screening Tool, a quick and simple way to determine if you may be at risk.
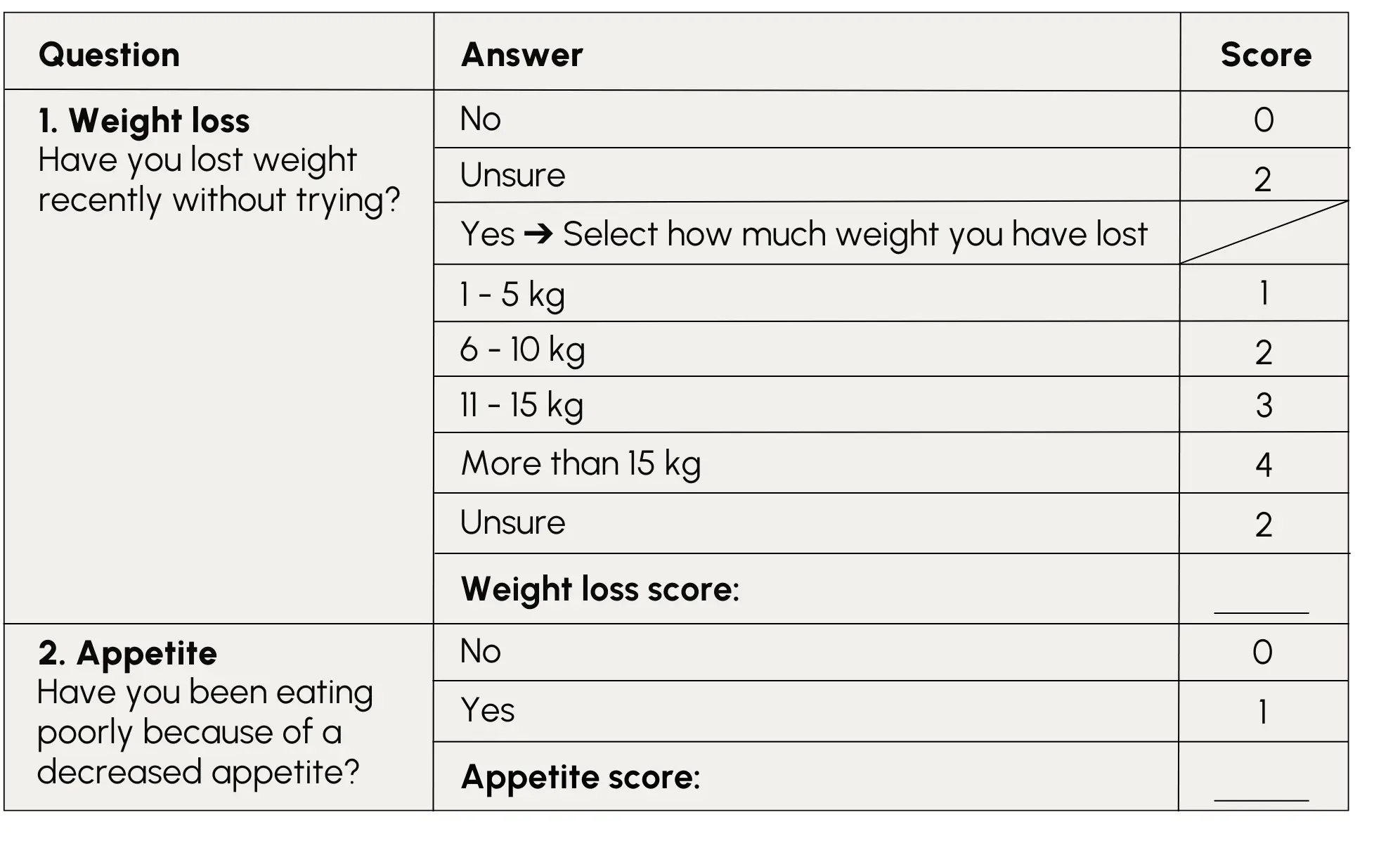
Malnutrition Screening Tool (MST)
Add your scores from Questions 1 and 2. A total score of 2 or more suggests you may be at risk of malnutrition and are strongly encouraged to speak to your doctor or dietitian.
Access nutritional support
Beyond the conditions highlighted above, our experienced team of dietitian provides comprehensive nutrition support tailored to a wide spectrum of health needs.
If you or your loved one could benefit from professional nutritional guidance, speak to your doctor for a referral or contact us to learn more about our dietetics services.
Let us help you take the next step toward better health - one meal at a time.
To make an appointment, call +65 6812 3781 or email parkway.dietetics@ihhhealthcare.com.
 Brain & Spine Care
Brain & Spine Care