-
-
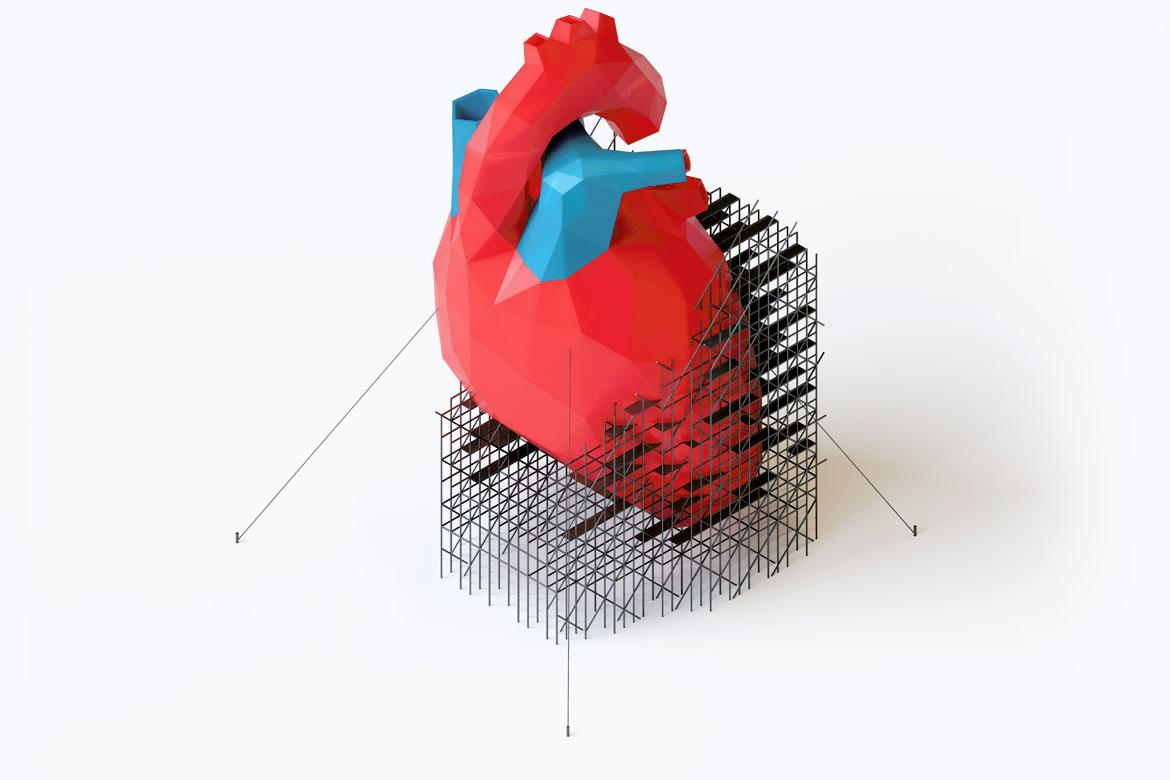
Featured Care Areas


Cardiology (Heart)
Related cardiovascular diseases
Cardiovascular disease is a general term that refers to heart and blood vessel conditions. Examples include:
Chronic heart disease
Chronic heart disease is a type of cardiovascular disease that affects your heart function repeatedly and over time. Examples of chronic heart diseases include:
- Coronary artery disease (CAD)
- Congenital heart disease (CHD)
- Heart arrhythmia (irregular heartbeat)
- Heart muscle disease (cardiomyopathy)
- Pulmonary arterial hypertension
- Valvular heart disease
- Heart failure
Heart conditions
Examples of heart conditions and diseases include:
- Angina
- Cardiac arrest
- Myocardial infarction (heart attack)
- Pleural effusion (fluid around lungs)
- Pregnancy-related cardiac conditions
- Valvular heart disease
Vascular conditions
Examples of blood vessel conditions include:
- Aortic aneurysm and aortic dissection
- Hypertension (high blood pressure)
- Pulmonary arterial hypertension
- Peripheral arterial disease
- Carotid artery disease
*This is not a complete list of all the conditions that are recognised and treated at our hospital. The information provided is for educational reference only and should not be seen as medical advice.
Please consult our qualified healthcare specialists for an accurate diagnosis before starting any treatment.
This page has been reviewed by our medical content reviewers.
Need help?
For enquiries, please call
+65 6250 0000 (Orchard) or +65 6898 6898 (Novena)
For appointment bookings, please WhatsApp
+65 8111 7777 (Orchard) or +65 8111 5777 (Novena)