We are pleased to announce that Mount Elizabeth Fertility Centre is now open at our new location at The Heeren.

Mount Elizabeth Fertility Centre
Our Services
At Mount Elizabeth Fertility Centre, we offer a comprehensive range of assisted reproductive technology (ART) services to help couples overcome a range of fertility issues and improve their chances of having a baby.
Assisted reproduction technology (ART) services
Our services include:
- Elective egg freezing (EEF)
- Ovulation induction and monitoring
- Intra-uterine insemination (IUI)
- Intracytoplasmic sperm injection (ICSI)
- In vitro fertilisation (IVF)
- Elective single blastocyst transfer
- Magnetic-activated cell sorting (MACS) system
- Pre-diagnostic sperm tests
- Surgical sperm retrieval for IVF programme
- Donor sperm programme (e.g. Fairfax Cyrobank, Xytex Sperm Bank, and Seattle Sperm Bank)
- Donor egg programme
MEFC donor sperm programme
Mount Elizabeth Fertility Centre's dedicated donor sperm programme assists couples who are unable to achieve pregnancy due to male infertility.
We will:
- Guide you through the process of selecting a sperm donor
- Handle the importation and shipment of the donor sperm
- Manage the storage of the frozen sperm specimens
Before undergoing treatment, you will go for a psychological counselling session with our counsellor. This session will help in your consideration and discuss the legal, social, genetic and moral aspects of conceiving a child from a sperm donor.
We work with 3 of the largest sperm banks in the United States. All sperm donors are screened for genetic diseases, chromosomal abnormalities and infectious diseases. These sperm banks are licensed and inspected by the Food and Drug Administration.
MEFC donor egg programme
Mount Elizabeth Fertility Centre works with one of the largest egg donor banks in Europe to import donor eggs.
To ensure the safety and quality of the donated oocytes (eggs):
- All egg donors undergo infectious disease and genetic testing screening
- The screening processes comply with the European Union Tissues and Cells Directive as well as Human Fertilisation & Embryology Authority's (HFEA) regulations on egg donation
When you are ready to embark on our donor egg programme, we will facilitate and coordinate with the overseas egg bank to handle all the shipping logistics for you.
Importing your frozen eggs, sperm or embryos from overseas
If you have eggs, sperm or embryos in storage overseas, it’s possible to move them into Singapore.
Our fertility team is able to assist you with the importation and transfer process, so that you can continue your assisted reproductive treatment with minimal interruption. We have worked with numerous medical couriers and Fertility Centers based in the United States, Europe and other Asian countries.
Overseas importation and transfer of frozen eggs, sperm and embryos are permitted by the Ministry of Health, Singapore.
Advanced fertility technologies
Our team of fertility specialists are up-to-date with the current IVF technologies and protocols, to provide comprehensive personalised care with ideal clinical outcomes. This includes preserving fertility of cancer patients prior to undergoing cancer treatment.
Read on to learn more about some of the advanced fertility technologies we employ.
Egg freezing, also known as oocyte cryopreservation, involves the extraction and preservation of a woman's eggs for future use.
The eggs are collected through a process known as ovarian stimulation, where hormone medications are administered to stimulate the ovaries to produce multiple eggs. Once the eggs have matured, they are retrieved and cryopreserved by rapidly cooling them to sub-zero temperatures. This freezing process halts biological activity, effectively preserving the eggs until they are ready to be used.
Egg freezing is an increasingly viable option for women who wish to delay childbearing for various reasons. In Singapore, egg freezing for medical reasons is allowed. From July 2023, elective egg freezing is also allowed for women aged 21 – 37, regardless of marital status.
Learn more about elective egg freezing below, or read our comprehensive guide to understand how it can benefit you.
Reasons for elective egg freezing
Cancer patients undergoing chemotherapy: Elective egg freezing offers a valuable opportunity for cancer patients who are about to undergo chemotherapy. Chemotherapy treatments can have detrimental effects on fertility, potentially compromising the ability to conceive in the future. By freezing their eggs before chemotherapy, cancer patients can safeguard their reproductive potential and increase the chances of starting a family after their treatment is completed.
Medical treatment that could affect fertility: Certain medical treatments, such as radiation therapy or surgical procedures, can have adverse effects on fertility. Elective egg freezing allows individuals undergoing such treatments to preserve their eggs for future use, mitigating the potential risks to their reproductive health.
Preserving younger eggs for future use: Elective egg freezing is an advantageous option for individuals who wish to preserve their fertility while they are still young. Women are born with a finite number of eggs, and as they age, the quantity and quality of these eggs naturally decline, making conception more challenging. By electively freezing their eggs at a younger age, individuals can effectively "pause" their biological clock and preserve the vitality of their eggs, ensuring a higher likelihood of successful pregnancies in the future.
Benefits for egg freezing
- Increased chances of future conception in family planning
- Flexibility to use eggs when ready
- Alleviates pressure and stress related to personal choices, priorities, lifestyle, career, and finances
- Provides more time to find the right partner and form a family
- Protects eggs from health conditions like cancer and treatments such as chemotherapy and radiation
Risks and complications for egg freezing
Failure to complete treatment as a result of:
- Poor follicular response
- Absence of eggs during oocyte retrieval
- Only mature eggs can be frozen
Operative risks as a result of:
- Infection
- Bleeding
Potential side effects of ovarian hyperstimulation syndrome (OHSS):
- Cramps / pain
- Swelling / bloat
- Hospitalisation / albumin infusions / abdominal tapping
Thaw survival rate:
- Approximately 90 – 97% of eggs survive the thawing process.
Risks for patients aged 45 and above:
- Increased risk of genetic abnormalities in the child
- Possible health or physical/mental impairments in the child due to advanced maternal age during pregnancy
- Considerations of physical and financial ability to care for the child until adulthood, taking into account the couple's health, older age, and the cost of raising a child as they grow older
- Potential impact of advanced parental age on the welfare of the child, including social acceptance, a large age gap between parents and the child, and the possibility of the child having to care for aged/ill parents or facing the loss of one or both parents during their schooling years or early in their careers
Our elective egg freezing services
At Mount Elizabeth Fertility Centre, our skilled fertility specialists have a wealth of experience in managing various fertility treatments including elective egg freezing.
Learn more about our bundles and fees for EEF services.
The EmbryoScope time-lapse system is an innovative technology that is used to closely monitor the development of embryos. It pairs with an incubator, a high resolution camera with an integrated computer software that can provide up to 135-hours, minute-by-minute microscopic video, documenting the growth of an embryo without disruption.
Benefits of EmbryoScope
The benefits of using an EmbryoScope include the following:
Reduced disruption and handling of embryos
Embryos incubated inside the EmbryoScope will never need to be removed for analysis thanks to the time-lapse system.
Comprehensive embryo analysis and monitoring
Development and key morphological features of embryos can be monitored by and analysed by embryologists via high quality images and video (up to 7,200 mins) captured by the built in camera. Anomalies that may not be visible during standard embryo culture can be shown in EmbryoScope.
Better embryo selection and ranking
In-depth and accurate data obtained via EmbryoScope provides comprehensive visual development of an embryo to aid in embryo selection and ranking. Our embryologists are able to identify the highest quality embryos for transfers or for cryopreservation and subsequently increase the chances of healthy pregnancies.
We provide sperm selection using magnetic-activated cell sorting (MACS) Annexin V system, which is designed to separate healthy sperm from those that have begun apoptosis (cell death) due to a high level of DNA fragmentation.
The purified sperm population shows a higher overall quality in terms of morphology, motility, DNA integrity and cryosurvival rate – thus yielding an improved sperm fertilisation potential and good embryo or blastocyst.
Benefits of MACS
MACS can benefit patients who have:
- Low fertilisation rate in previous cycles
- Poor embryo quality in previous cycles
- Abnormal sperm parameters
- Varicocele (enlargement of the veins within the scrotum)
- Cancer, by preserving fertility before or after chemotherapy or radiotherapy
Beyond the parameters that we look at in a normal semen analysis, there are other diagnostic tests that can provide more insights into sperm health.
These tests include:
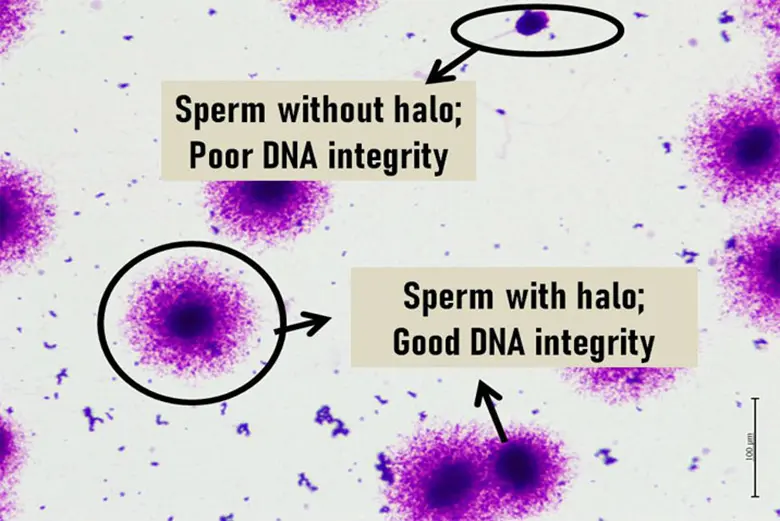
DNA fragmentation test
DNA fragmentation of sperm correlates to the integrity of the genetic material in sperm, and high DNA fragmentation can be an explanation for infertility, recurrent miscarriages and poor IVF outcomes.
The major contributing factor for high DNA fragmentation is oxidative stress associated with advanced chronological age, alcohol, diet, increased testicular temperature, infection, occupational pollutants, smoking, stress and varicocele (an enlargement of the veins within the scrotum).
A DNA fragmentation test can provide a reliable sperm analysis at a molecular level by detecting abnormal genetic material within the sperm, which in turn helps to identify men who are at risk of subfertility.
Hyaluronan binding assay (HBA)
Hyaluronan binding assay (HBA) assesses the maturity of sperm. Hyaluronan (HA) is a sugar molecular surrounding the egg and only mature sperm can bind to it. Sperm that binds to HA have enhanced levels of developmental sperm maturity, including fewer chromosomal abnormalities and higher sperm DNA integrity.
The HBA test is another component of the sperm analysis that is reliable in the diagnosis of suspected male infertility, to predict sperm performance and fertilisation potential.
Oxisperm test
The Oxisperm test assesses the oxidative stress levels of sperm. High level of oxidative stress in sperm indicate an elevated level of reactive oxygen species (ROS), which have a direct negative impact on sperm DNA integrity and motility. Exposure to substances such as tobacco, alcohol, household appliances, radiation (from laptops, TV and UV rays), and heavy metals can lead to elevated levels of ROS.
Oxidative stress refers to an imbalance between the generation of ROS and the body’s ability to neutralise their harmful effects through antioxidants. Sperm is highly susceptible to oxidative stress and when in this state, peroxidative damage will be induced in sperm plasma membrane resulting in DNA fragmentation.
High oxidative stress has been associated with poor sperm motility and function, leading to poor embryo formation, miscarriage, and infertility. Conditions such as varicoceles, infection, inflammation, and spinal cord injury, have also been associated with oxidative stress-induced infertility.
These pre-diagnostic tests provide information that can help in clinical diagnosis, management and treatment of male fertility, and increase favourable outcome for assisted reproduction procedures.
Patients who may benefit from these tests may have indicating factors such as:
- Advanced chronological age
- Multiple failed IVF/ICSI treatments
- Poor blastocyst development
- Recurrent miscarriage
- Unexplained infertility
- Varicocele
Our strict laboratory standards with ideal culture conditions allow us to support the growth of embryos to the blastocyst stage.
Our ability to develop embryos to the blastocyst stage allows us to select the healthiest embryos with the highest potential for implantation at the time of transfer.
Only 1 or 2 blastocysts will be transferred, versus the traditional transfer of 3 or 4 early-stage embryos, back to the mother. This reduces the risk of multiple births from IVF, while improving pregnancy rates.
Our chief embryologist, Ms Ng Lai Cheng, has been culturing blastocysts since 1993, first as part of an animal research co-culture team in blastocyst culture and transfer and later on in clinical embryology.
Patients with poor ovarian response while undergoing IVF treatment can have renewed hope with the double stimulation protocol. Poor ovarian response could be due to multiple factors, including diminished ovarian reserves or older age.
In classic IVF procedures, only 1 oocyte retrieval (egg collection) is performed using mild ovarian stimulation during the early follicular phase of the menstrual cycle. In the double stimulation protocol, a second oocyte retrieval is performed during the luteal phase.
Double stimulations are performed during both the follicular and luteal phases in the same menstrual cycle, leading to higher opportunity to retrieve more oocytes. This allows for better chances in obtaining quality blastocysts and therefore higher pregnancy success rates.
We routinely apply a laboratory technique known as freeze-all IVF, which gives couples more options than before.
Vitrification is a method for the safe freezing of blastocysts. It avoids the formation of ice crystals, which can be extremely damaging to frozen embryos.
Vitrification in IVF allows for better survival rates of thawed embryos and improved pregnancy rates after frozen transfer procedures. This translates to better pregnancy outcomes and a lowered chance of obstetric complications such as pre-term labour or foetal growth restriction.
Quality blastocysts (advanced day 5 or day 6 embryos) that remain after the end of a treatment cycle will be saved, via vitrification, for future use.
The freeze-all blastocysts strategy is especially beneficial for women who:
- Are diagnosed with low ovarian reserves
- Encounter poor ovarian response during IVF treatment
- Are older
- Are cancer patients who wish to preserve their fertility prior to undergoing cancer treatments
In this section
 Brain & Spine Care
Brain & Spine Care